For decades, genetic research moved at the pace of manual lab work - pipetting samples, running gels, waiting weeks for results. Today, that’s all changed. Artificial intelligence isn’t just speeding things up; it’s rewriting the rules of how we understand DNA. Scientists now use AI to find hidden patterns in billions of genetic letters that no human could ever spot on their own. This isn’t science fiction. It’s happening in labs right now, from Boston to Minneapolis, and it’s changing how we diagnose diseases, predict risks, and even design treatments.
What AI Actually Does in Genetic Research
At its core, AI in genetics is about finding signals in noise. Your genome has about 3 billion base pairs. Most of them don’t change between people. But the tiny fraction that does - a few million variations - can mean the difference between staying healthy and developing a disease. AI tools like deep learning models scan through these variations, looking for connections to conditions like cancer, Alzheimer’s, or rare inherited disorders.
One example: researchers at the Broad Institute trained a neural network on over 500,000 whole-genome sequences. The model learned to predict which non-coding regions - areas once called "junk DNA" - actually regulate gene activity. It found 12,000 new regulatory switches that had been missed by traditional methods. That’s not just a technical win. It means doctors could soon test for risk factors in parts of the genome we didn’t even know mattered.
From Sequencing to Diagnosis: Faster, Smarter
Sequencing a human genome used to cost $100 million and take years. Now, it’s under $600 and done in a day. But having the data doesn’t mean you understand it. That’s where AI steps in.
Tools like DeepVariant, developed by Google Health, use convolutional neural networks to read sequencing data and call genetic variants with 99.9% accuracy - better than most human analysts. In a 2024 study published in Nature Genetics, DeepVariant reduced false positives in cancer genome tests by 40% compared to older software. That means fewer patients get wrongly told they have a dangerous mutation, and fewer get missed entirely.
Hospitals in the U.S. and Europe are now using AI-powered diagnostic tools to analyze tumor DNA within hours of biopsy. Instead of waiting weeks for a genetic report, oncologists get actionable insights in under 24 hours. For patients with aggressive cancers, that time difference can be life-or-death.
Discovering New Genes and Drug Targets
Before AI, finding a disease-linked gene was like finding one specific book in a library the size of the Amazon. Researchers would study families with inherited conditions, track who got sick, and hope for patterns. It took years. Sometimes decades.
Now, AI models like AlphaFold and its newer cousin, RoseTTAFold, predict how proteins fold based on genetic code. Why does that matter? Because most diseases happen when proteins misfold. If you can predict how a mutation changes a protein’s shape, you can guess whether it’s harmful - even if no one’s ever seen that mutation before.
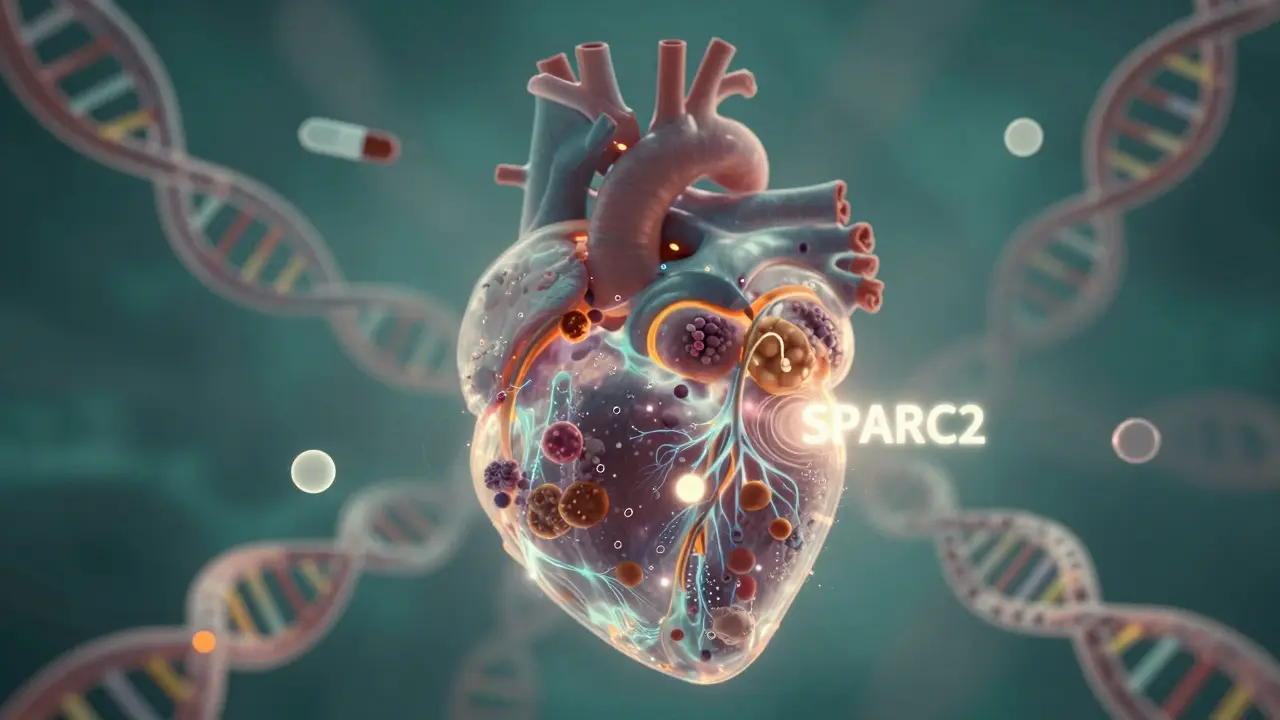
In 2025, a team at the University of California used AI to scan 2 million genomes from the UK Biobank. They identified 87 new gene variants linked to heart disease, 32 of which had never been reported. One of them, a gene called SPARC2, turned out to affect cholesterol clearance. Drug companies are now testing new therapies targeting SPARC2. Without AI, this gene might have stayed hidden for another 20 years.
Personalized Medicine Gets Real
Two people can have the same cancer - say, breast cancer - and respond completely differently to the same drug. Why? Because their genomes are different. AI helps untangle that.
Companies like Tempus and Foundation Medicine now combine tumor sequencing with AI to build individualized treatment plans. Their systems look at hundreds of genetic markers, plus lifestyle data and past treatment history, to recommend which therapy has the highest chance of working. In a real-world trial at Mayo Clinic, patients whose treatment was guided by AI had a 35% higher response rate than those treated with standard protocols.
This isn’t just for cancer. AI is helping tailor treatments for rare diseases like Duchenne muscular dystrophy and Huntington’s. For kids born with genetic disorders that used to mean a short life expectancy, AI-driven therapies are now extending survival by decades.
Challenges and Ethical Risks
It’s not all breakthroughs. AI in genetics has serious downsides.
First, bias. Most genomic data comes from people of European descent. AI models trained on that data perform poorly for African, Asian, or Indigenous populations. In one 2024 study, a widely used AI tool misclassified pathogenic variants in Black patients 2.5 times more often than in white patients. That’s not just a technical flaw - it’s a health inequity.
Second, privacy. Your genome is the most personal data you have. Once it’s in a database, it can’t be changed like a password. AI systems that analyze DNA are often run by private companies. Who owns that data? Can insurers use it? Can employers? There are no clear laws yet.
And then there’s the "black box" problem. AI can tell you a mutation is dangerous - but not always why. Doctors need to explain risks to patients. If they can’t explain how the AI reached its conclusion, trust breaks down.
The Future: AI and Human Expertise Together
The best genetic research today doesn’t replace scientists - it empowers them. AI handles the massive data crunching. Humans interpret the results, ask the right questions, and make ethical calls.
At the University of Minnesota’s Genomics Center, researchers use AI to flag potential disease-causing variants, then human geneticists review them. The AI cuts down the review time from 30 hours to 4. That means genetic counselors can spend more time talking to patients instead of staring at screens.
The next big leap? AI that predicts not just disease risk, but how someone will respond to a drug, a diet, or even a vaccine - all based on their unique genome. We’re not there yet. But in labs across the U.S., that future is being built, one algorithm at a time.
Can AI predict genetic diseases before symptoms appear?
Yes, but with limits. AI can analyze your genome and estimate your risk for conditions like type 2 diabetes, heart disease, or certain cancers. For example, a polygenic risk score - built using AI on millions of genetic markers - can tell you if you’re in the top 5% of risk for coronary artery disease. But risk isn’t destiny. Lifestyle, environment, and random chance still play huge roles. AI gives you a heads-up, not a guarantee.
Is AI better than human geneticists at reading DNA?
Not better - better together. AI processes data faster and spots patterns humans miss. But human experts understand context. A variant might look dangerous in a database, but if it’s common in a healthy population, it’s probably harmless. AI can’t make that call alone. That’s why top labs now use AI as a first filter, then rely on geneticists to confirm findings. The most accurate results come from this teamwork.
How accurate are AI tools in diagnosing rare genetic disorders?
For rare disorders, AI has cut diagnostic delays from years to days. In a 2023 trial involving 1,200 children with undiagnosed conditions, an AI tool called WGS-Analyzer correctly identified the genetic cause in 43% of cases within 72 hours. Before AI, the average time to diagnosis was over 4 years. For families with a sick child, that speed is priceless. Accuracy varies by disorder, but for conditions like Rett syndrome or spinal muscular atrophy, AI now matches or exceeds expert human analysis.
Does AI use my DNA data without my permission?
Legally, no - but the rules are patchy. In the U.S., the Genetic Information Nondiscrimination Act (GINA) stops employers and health insurers from using genetic data against you. But it doesn’t cover life insurance, long-term care, or companies selling DNA tests. If you upload your genome to a private company, they might use it to train their AI - even if you didn’t sign up for that. Always read the fine print. Opt-in consent is still the best protection.
Will AI replace genetic counselors?
No. Genetic counselors are trained to explain complex risks, handle emotional reactions, and guide decisions. AI can tell you you’re at high risk for a disease. It can’t help you decide whether to tell your siblings, whether to have kids, or how to cope with the news. That’s human work. AI is a tool - not a replacement. In fact, as AI makes genetic testing more common, the need for counselors is growing, not shrinking.

